Testosterone Replacement Therapy In Delhi, India
Testosterone is a crucial steroid hormone from the androgen group responsible for various physiological functions in men. It plays a vital role in developing male secondary sexual characteristics, muscle mass, bone density, and overall well-being. Testosterone deficiency, or hypogonadism, is a global men’s health concern, affecting various aspects of health including sexual function, cardiovascular health, and mental well-being.
New Delhi Andrology Clinic, India’s leading men’s health clinic, specializes in Testosterone Replacement Therapy (TRT) under the expert guidance of Dr. Vijayant Govinda Gupta. We offer comprehensive TRT solutions, ranging from oral medications to injectable testosterone therapies.
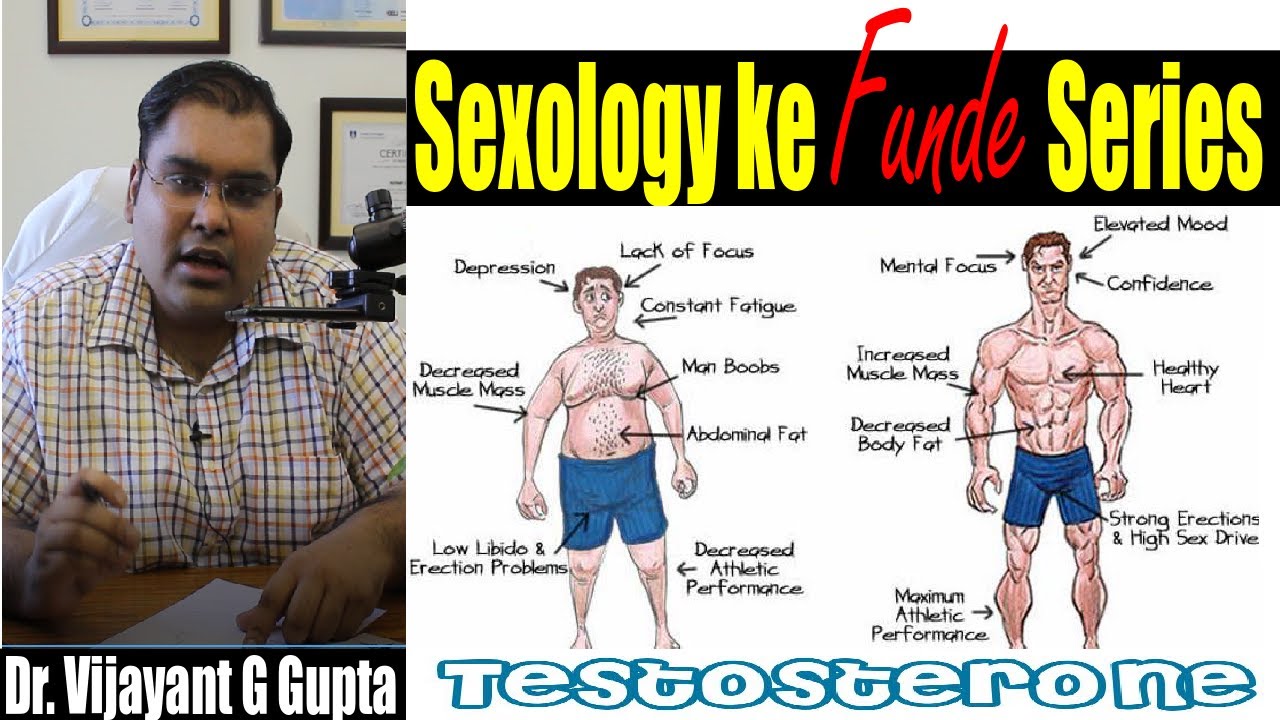
Symptoms and Signs of Low Testosterone
Men with low testosterone may experience:
Reduced energy and endurance
Mood swings, irritability, and depression
Cognitive issues such as poor concentration and memory
Loss of lean muscle mass and increased fat accumulation
Reduced libido and erectile dysfunction
Weak bones leading to osteoporosis
Increased risk of cardiovascular diseases
Diagnosing Low Testosterone
The American Urological Association (AUA) recommends that clinicians use a total testosterone level below 300 ng/dL as a diagnostic threshold for low testosterone.
Testosterone levels should be measured twice on separate occasions in the early morning for accurate diagnosis.
Additional tests such as serum luteinizing hormone (LH), prolactin, estradiol, PSA levels, and hematocrit levels are advised before starting TRT.
Benefits of Testosterone Replacement Therapy (TRT)
Scientific evidence suggests that testosterone replacement therapy offers multiple benefits, including:
Improved body composition: TRT helps increase lean muscle mass and reduce fat. A study analyzing 12 clinical trials found that lean body mass increased by 1.9 kg with testosterone therapy.
Stronger bones: Men undergoing TRT for 24 months showed a 3-4% increase in bone mineral density (BMD) at the lumbar spine and femoral neck.
Enhanced libido and sexual function: Testosterone levels naturally rise in response to sexual arousal, and TRT can improve libido and erectile function.
Better cardiovascular health: Studies indicate that low testosterone levels are linked to an increased incidence of major adverse cardiac events (MACE), hypertension, and myocardial infarction.
Mental well-being: TRT may reduce depression, improve cognitive function, and enhance overall mood.
Monitoring and Safety of TRT
Regular monitoring is crucial for optimizing therapy and minimizing risks. Key assessments include:
Symptom evaluation every 3 months
Total Testosterone levels every 3 months
Hemoglobin and Hematocrit levels to prevent polycythemia
Liver function tests (LFTs)
Prostate-Specific Antigen (PSA) tests every 6 months in men over 40
Blood pressure, weight, and blood sugar monitoring
Potential Risks and Considerations
Cardiovascular Risks and TRT
The FDA issued a warning regarding a potential link between TRT and cardiovascular events. However, large observational studies did not find conclusive evidence of increased cardiovascular risk. The AUA guidelines emphasize that TRT should be avoided for 3-6 months post-cardiovascular event.
VTE (Venothrombolic Events) and TRT
Concerns about TRT and venous thromboembolism (VTE) led the FDA to mandate warning labels on testosterone products. However, four large observational studies (Baillargeon et al., Sharma et al.) found no association between TRT and increased VTE risk.
Prostate Cancer and TRT
While the FDA retains a warning about potential prostate cancer risk in patients using TRT, current evidence does not support a direct link. A meta-analysis of 7 randomized controlled trials (RCTs) found no significant increase in prostate cancer incidence in older men receiving TRT compared to placebo.
Studies supporting these findings include:
Steidle et al. (2003): Testosterone gel improves androgen levels without increasing prostate cancer risk.
Srinivas-Shankar et al. (2010): TRT enhances muscle strength and quality of life in elderly men.
O’Connell et al. (2011): TRT benefits persist even 6 months after discontinuation.
Who Should Avoid TRT?
Men actively trying to conceive (Exogenous testosterone suppresses sperm production.)
Men with untreated sleep apnea or severe cardiovascular conditions
Patients with uncontrolled polycythemia
Men with active prostate or breast cancer
Video on Testosterone Replacement Therapy
Playlist
FAQs About Testosterone Replacement Therapy (TRT)
Yes, when properly monitored, TRT is safe and beneficial. Regular medical check-ups are essential to minimize potential risks.
Improvements in energy levels and mood may be noticeable within weeks, while significant changes in body composition and libido typically occur over months.
Yes, TRT can enhance libido and erectile function, but it may not be a complete solution for all cases of ED.
TRT can aid in reducing fat mass and increasing muscle mass, but a healthy diet and exercise remain essential.
Yes, exogenous testosterone can suppress sperm production. Men planning to conceive should discuss alternatives with their doctor.
TRT may be long-term depending on the cause of testosterone deficiency. Your doctor will determine the best approach based on your individual needs.
Coverage varies by insurance provider. It is best to check with your insurer for specific details.
Testosterone Replacement Therapy (TRT) in India is a transformative treatment for men suffering from testosterone deficiency. While concerns about TRT-related risks exist, current scientific evidence overwhelmingly supports its benefits in improving quality of life, cardiovascular health, sexual function, and mental well-being.
At New Delhi Andrology Clinic, Dr. Vijayant Govinda Gupta offers expert consultation and customized TRT solutions to help men achieve optimal hormonal balance and health.
For consultations on TRT in India, book an appointment today with Dr. Vijayant Govinda Gupta.
References
Baillargeon J, Urban RJ, Morgentaler A et al: Risk of venous thromboembolism in men receiving testosterone therapy. Mayo Clin Proc 2015; 90: 1038.
Sharma R, Oni OA, Chen G et al: Association between testosterone replacement therapy and incidence of DVT and pulmonary embolism: Chest 2016; 150: 563.
Steidle C, Schwartz S, Jacoby K et al: Testosterone gel normalizes androgen levels in aging males. J Clin Endocrinol Metab 2003; 88: 2673.
Srinivas-Shankar U, Roberts SA, Connolly MJ et al: Effects of testosterone on muscle strength, body composition, and quality of life. J Clin Endocrinol Metab 2010; 95: 639.
O’Connell MD, Roberts SA, Srinivas-Shankar U et al: Do testosterone effects persist after treatment? J Clin Endocrinol Metab 2011; 96: 454.
Testosterone Replacement Therapy (TRT) in India is a transformative treatment for men suffering from testosterone deficiency. While concerns about TRT-related risks exist, current scientific evidence overwhelmingly supports its benefits in improving quality of life, cardiovascular health, sexual function, and mental well-being.
At New Delhi Andrology Clinic, Dr. Vijayant Govinda Gupta offers expert consultation and customized TRT solutions to help men achieve optimal hormonal balance and health. For consultations on TRT in India, book an appointment today with Dr. Vijayant Govinda Gupta.
Precaution on Testosterone Replacement
Cardiovascular
Hypertension
Venous Thrombosis
Prostate
Fertility
Major Adverse Cardiac Events (MACE) On TRT
There is maybe association between testosterone therapy and subsequent MACE events nor can it be stated definitely that testosterone therapy is associated with reduced incidence of MACE.
However, the FDA added a warning to testosterone product labeling after reviewing five observational studies and two meta-analyses of RCTs that examined the effects of testosterone therapy on MACE.
VTE (Venothrombolic Events) On TRT
The concern about the possible association between testosterone therapy and venothrombolic events (VTE) led the FDA to require pharmaceutical companies to add a warning to their product labeling regarding postmarketing reports of VTE;
Since the FDA warning in June 2014, four large observational studies198, 359-361 have been conducted, none of which showed an association between testosterone therapy and an increased risk of VTE.
Baillargeon J, Urban RJ, Morgentaler A et al: Risk of venous thromboembolism in men receiving testosterone therapy. Mayo Clin Proc 2015; 90: 1038.
Sharma R, Oni OA, Chen G et al: Association between testosterone replacement therapy and the incidence of DVT and pulmonary embolism: a retrospective cohort study of the veterans administration database. Chest 2016; 150: 563.
References
Prostate Cancer And Testosterone Replacement Therapy in India
While the FDA retains a warning regarding the potential risk of prostate cancer in patients who are prescribed testosterone products (“patients treated with androgens may be at increased risk for prostate cancer”)
there is accumulating evidence against a link between testosterone therapy and prostate cancer development.
A meta-analysis of 7 RCTs showed that there was no significant increase in the rate of a prostate cancer diagnosis in older, testosterone deficient men who were treated with testosterone compared to placebo
Steidle C, Schwartz S, Jacoby K et al: AA2500 testosterone gel normalizes androgen levels in aging males with improvements in body composition and sexual function. J Clin Endocrinol Metab 2003; 88: 2673.
Srinivas-Shankar U, Roberts SA, Connolly MJ et al: Effects of testosterone on muscle strength, physical function, body composition, and quality of life in intermediate-frail and frail elderly men: a randomized, double-blind, placebo controlled study. J Clin Endocrinol Metab 2010; 95: 639.
O’Connell MD, Roberts SA, Srinivas-Shankar U et al: Do the effects of testosterone on muscle strength, physical function, body composition, and quality of life persist six months after treatment in intermediate-frail and frail elderly men? J Clin Endocrinol Metab 2011; 96: 454.
References